The Infected Blood Scandal stands as a tragic chapter in medical history, marked by profound human suffering, institutional failures, and a quest for justice and accountability. More than 30,000 people, including children, were infected with viruses such as HIV and hepatitis after being given tainted blood between the 1970s and early 1990s.
A bombshell report released Monday found that the tainted blood affair was covered up by successive governments and health officials and largely could have been avoided. Prime Minister Rishi Sunak issued a “wholehearted and unequivocal” apology and promised compensation for everyone affected.
Key Points to Know About the Infected Blood Scandal
1. Scope and Impact
The scandal unfolded in the 1970s and 1980s when thousands of patients in the United Kingdom were infected with HIV and hepatitis C through contaminated blood products. It’s estimated that over 4,000 people were affected, many of whom were haemophiliacs or received blood transfusions.
2. Contaminated Blood Products
The primary cause of the scandal was the use of blood products sourced from high-risk donors, including prisoners, drug users, and paid donors. These products were not properly screened for infections, leading to widespread transmission of HIV and hepatitis C.
3. Haemophilia Community Impact
Haemophiliacs were disproportionately affected due to their reliance on blood products for clotting factor replacement therapy. Many were infected with HIV and hepatitis C, leading to severe illness, premature death, and significant psychological trauma for patients and their families.
4. Government Involvement
Government agencies and health authorities were implicated for their role in the procurement, regulation, and distribution of contaminated blood products. Criticisms include negligence, inadequate safety protocols, and a lack of transparency and accountability.
5. Delayed Response
Despite early warnings and evidence of contamination, authorities failed to take timely action to address the risks and protect patients. Delays in implementing screening measures and withdrawing contaminated products exacerbated the spread of infections and contributed to the scale of the tragedy.
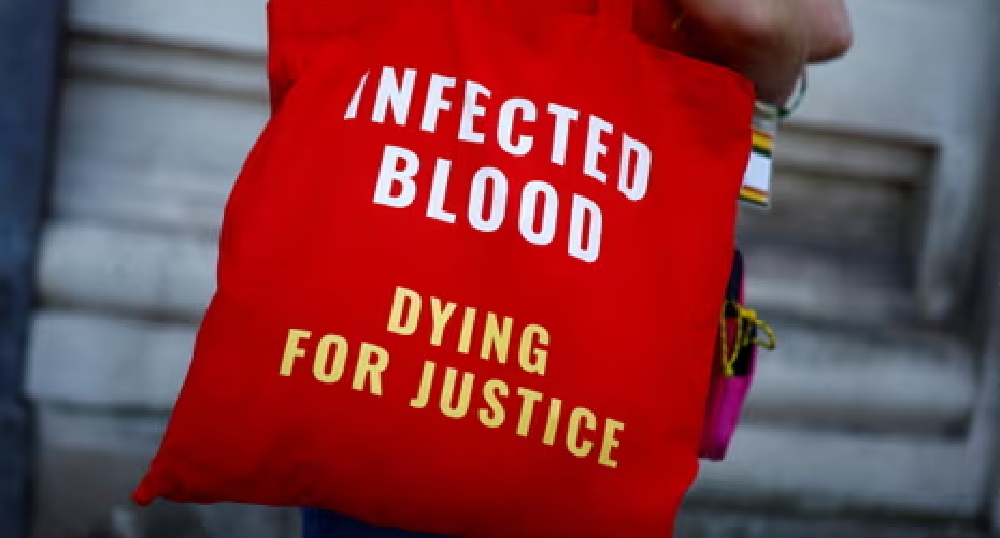
6. Campaign for Justice
Survivors, families of victims, and advocacy groups have long campaigned for justice, accountability, and compensation. Their efforts have led to inquiries, legal proceedings, and calls for government apologies and reparations.
7. Inquiry and Investigations
In 2017, the United Kingdom launched the Infected Blood Inquiry, a public inquiry tasked with examining the causes, scale, and impact of the scandal. The inquiry aims to uncover the truth, hold accountable those responsible, and provide closure and support to affected individuals and communities.
8. Medical and Ethical Failures
The scandal exposed systemic failures in the healthcare system, including inadequate regulation, ethical lapses, and a disregard for patient safety. It raised questions about medical ethics, informed consent, and the responsibility of healthcare providers to prioritize patient welfare.
9. Legacy and Lessons
The legacy of the scandal endures as a reminder of the human cost of negligence and incompetence in healthcare. It underscores the importance of robust safety protocols, transparency, and accountability in medical practice and public health policy.
10. Ongoing Impact
Despite decades having passed since the scandal, its impact continues to reverberate within affected communities. Many survivors still grapple with health complications, stigma, and the emotional toll of their experiences. Efforts to address the long-term needs of survivors and provide support and redress remain ongoing.