Health
70% of women with polycystic ovary syndrome not aware – Gynaecologist
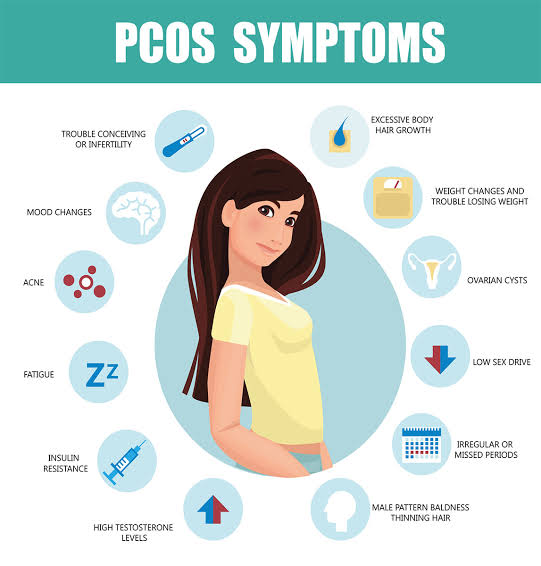
*Says, they risk infertility
By Francesca Hangeior.
As the world commemorates this year’s Polycystic Ovary Syndrome Awareness Month, a fertility specialist, Dr. Abayomi Ajayi, has said about 70 percent of women living with the condition are not aware that they have it due to ignorance.
PCOS is a common hormonal condition that affects women of reproductive age.
Ajayi, who is Medical Director, Nordica Fertility Centre, Lagos, said PCOS was a prevalent cause of infertility, especially anovulatory infertility.
He also stated that PCOS was the most common cause of hormonal disorders in women of reproductive age, causing disrupted ovulation and a lack of regular menstruation.
The consultant gynaecologist disclosed this during a webinar organised by the fertility centre to commemorate this year’s PCOS awareness month aimed at raising awareness about the condition.
PCOS Awareness Month is a global healthcare event observed annually throughout September. It aims to improve the lives of those affected by the condition, help them overcome their symptoms, and prevent and reduce their risks for life-threatening diseases such as diabetes.
The World Health Organisation says PCOS affects an estimated eight to 13 per cent of reproductive-aged women.
The global health body also states that up to 70 percent of women with the condition remain undiagnosed worldwide despite being a leading cause of infertility.
“PCOS is a common hormonal condition that affects women of reproductive age. It usually starts during adolescence, but symptoms may fluctuate over time.
“PCOS can cause hormonal imbalances, irregular periods, excess androgen levels, and cysts in the ovaries. Irregular periods, usually with a lack of ovulation, can make it difficult to become pregnant.
“PCOS is a chronic condition and cannot be cured. However, some symptoms can be improved through lifestyle changes, medications, and fertility treatments”, the WHO said.
Ajayi pointed out that the exact cause of PCOS was unknown, adding however that the condition could be genetic.
The consultant gynaecologist said, “September is PCOS awareness month, and that is why we have gathered here today to dispel the myths about PCOS, raise awareness, and offer support to women who are living with the condition so that we can empower them to take care of their health.
“PCOS has no cure, so it is something that they are going to live with for the rest of their lives. So they should understand it. It is a common abnormality in women, and it is a common cause of infertility, especially anovulatory infertility.
“It is estimated that 10 to 15 percent of women will have PCOs. Unfortunately, about 50 to 70 percent of them will not be diagnosed. So, there are still a lot of misdiagnoses and underdiagnoses going on.”
He noted that due to misdiagnoses, a lot of women were labeled to have PCOS when they were not, and the people who had PÇOs were not diagnosed most of the time.
“So, we must talk about this and ask questions. Why are we having misdiagnosis? We have this because people rely on laboratory results and that might not be true. Two out of three symptoms must be present before diagnosis of PCOS is done”, he said.
According to him, symptoms vary from woman to woman, with some experiencing milder symptoms and others more severe.
“Symptoms are linked to hormones, with women with PCOS having slightly higher testosterone levels, leading to facial hair growth, and insulin resistance, a condition where the body doesn’t respond to insulin, increasing glucose levels and leading to weight gain and fertility issues”, he added.
The maternal health expert explained that the treatment for PCOS and infertility often begins with an ultrasound diagnosis, which helps determine the necessary tests.
“Physical examinations, including height, weight, facial or body hair growth, acne, and discoloration of the skin under the arms, breasts, and groin, can help diagnosis. Insulin resistance, common to PCOS, may play a role in weight gain and the difficulty of losing any extra weight.
“With fertility medications, the chances of getting pregnant with PCOS are quite favorable. Although there is currently no cure for PCOS, some women’s periods do normalize after birth, and those with fertility issues may find it easier to conceive again. IVF is an excellent choice, but its effectiveness depends on individual factors such as age, length of infertility, and weight.
“Many women with PCOS suffer from physical or psychological manifestations of depression, which should be sought by a doctor who is willing to listen to concerns and not dismiss this potential side effect of PCOS,” Ajayi said.
He advised women with the condition to see a maternal health specialist for proper evaluation and appropriate treatment.
“Women with PCOS need a proper evaluation of infertility. If the cause is just PCOS, they will do ovulation induction with drugs and drugs are available.
Health
SAD! Lassa Fever Claims 127 Lives Across 18 States in Nigeria(List)

The Nigeria Centre for Disease Control and Prevention (NCDC) has reported a sharp rise in Lassa fever cases, with 127 deaths confirmed across 18 states as of April 6, 2025.
According to the agency’s latest situation report, 674 people have tested positive for the virus out of 4,025 suspected cases recorded between January and early April.
The current Case Fatality Rate (CFR) stands at 18.8%, slightly higher than the 18.5% recorded during the same period in 2024, indicating a worrying upward trend.
The most affected states include Taraba (31 deaths), Ondo (26), Edo (17), Bauchi (12), and Ebonyi (11). Other states with reported fatalities are Gombe (7), Kogi (4), Benue (4), Nasarawa (4), Plateau (5), Kaduna (2), and one death each in Enugu, Delta, Cross River, and Ogun.
The report also highlights that 71% of confirmed cases were concentrated in Ondo (30%), Bauchi (25%), and Edo (16%), with the remaining 29% spread across 15 other states. The virus has now reached 93 local government areas nationwide.
Lassa fever is a viral haemorrhagic illness transmitted mainly through exposure to food or household items contaminated by infected rodents, particularly the multimammate rat. It can also spread through direct contact with the blood, urine, feces, or other bodily secretions of an infected person.
The disease predominantly affects people between the ages of 21 and 30, with a male-to-female ratio of 1:0.8, according to NCDC data.
In response to the outbreak, the NCDC has activated the National Lassa Fever Multi-Partner, Multi-sectoral Incident Management System to strengthen surveillance, case management, risk communication, and coordination efforts at all levels.
As the country continues to battle the spread of the virus, the NCDC is urging citizens to maintain proper hygiene, store food in rodent-proof containers, and seek immediate medical attention if symptoms such as fever, headache, sore throat, chest pain, or vomiting occur
Health
FG identifies 1,277 persons for monitoring as Lassa fever kills 122

The Nigeria Centre for Disease Control and Prevention has listed 1,277 persons for follow-up over the possibility of being infected with Lassa fever. This follows the centre recording 659 confirmed cases out of 3,779 suspected cases and 122 deaths in 13 weeks (from January to March 30, 2025).
A report obtained from the NCDC on Friday indicated that no fewer than 18 states across the country have recorded Lassa fever cases, with Ondo, Bauchi, and Edo being the most affected.
The report partly reads, “Cumulatively, in week 13 of 2025, 122 deaths have been reported, with a Case Fatality Rate of 18.5%, which is lower than the CFR for the same period in 2024 (18.7%).
“In total for 2025, 18 states have recorded at least one confirmed case across 93 Local Government Areas. Seventy-one per cent of all confirmed Lassa fever cases were reported from these three states (Ondo, Bauchi, and Edo), while 29% were reported from 15 other states with confirmed Lassa fever cases. Of the 71% of confirmed cases, Ondo reported 30%, Bauchi 25%, and Edo 16%.
“The predominant age group affected is 21-30 years (Range: 1 to 94 years, Median Age: 30 years). The male-to-female ratio for confirmed cases is 1:0.8. The number of suspected cases increased compared to that reported for the same period in 2024. No new healthcare worker was affected in week 13. The National Lassa fever multi-partner, multi-sectoral Incident Management System (IMS) was activated to coordinate the response activities at all levels.”
The report shows that the contacts under follow-up number 1,277, while the contacts that have completed follow-up total 1,448.
According to the NCDC, the disease has affected 20 healthcare workers in eight states so far this year.
Lassa fever is an acute viral haemorrhagic fever caused by the Lassa virus. The natural reservoir for the virus is the multimammate rat (also known as the African rat), although other rodents can also act as carriers.
The public health institute stated that Lassa fever cases occur year-round, with peak transmission periods typically from October to May.
Health
WHO calls for countries to address disruptions to TB services
In the wake of massive cuts in US funding, the World Health Organization (WHO) today called on global health leaders, donors, and policymakers to protect and maintain tuberculosis (TB) care and support services around the world.
In a statement issued ahead of World Tuberculosis Day (March 24), the WHO said the “drastic and abrupt” cuts to global health funding threaten to reverse gains made in global efforts to combat TB, which remains the world’s deadliest infectious disease. Those efforts have saved an estimated 79 million lives worldwide since 2000, the organization said.
“The huge gains the world has made against TB over the past 20 years are now at risk as cuts to funding start to disrupt access to services for prevention, screening, and treatment for people with TB,” said WHO Director-General Tedros Adhanom Ghebreyesus, PhD. “But we cannot give up on the concrete commitments that world leaders made at the UN General Assembly just 18 months ago to accelerate work to end TB. WHO is committed to working with all donors, partners and affected countries to mitigate the impact of funding cuts and find innovative solutions.”
USAID cuts have crippled TB control efforts
While the statement does not specifically mention the US Agency for International Development (USAID), the Trump administration’s freeze of USAID funding, and the subsequent canceling of thousands of contracts issued by the agency, have left a gaping hole in funding for TB prevention, screening, and treatment services. The US government has been the leading bilateral donor to global TB control efforts, contributing $200 million to $250 million annually—roughly one quarter of international donor funding for the disease.
The WHO said 27 countries are facing crippling breakdowns in their TB response, with the biggest impact seen in high-TB burden countries in Africa, Southeast Asia, and the Western Pacific. Among the services that have been disrupted are diagnosis, active case finding, screening, and contact tracing, and those disruptions are resulting in delayed detection and treatment and increased transmission risk. Drug supply chains, laboratory services, and data and surveillance systems have also been undermined.
A recent update from StopTB Partnership, which works on TB response with more than 2,000 partners in 100 countries, provides some detail on the services affected by the USAID funding cuts. In Cambodia, active case finding has halted in half the country, resulting in 100,000 people missing TB screening and 10,000 cases of drug-susceptible (DS)-TB going undetected. In Kenya, sputum sample transport once supported by USAID has halted, affecting the diagnosis of DS- and drug-resistant (DR)-TB. In India, USAID-funded TB screening projects in vulnerable groups have stopped.
The huge gains the world has made against TB over the past 20 years are now at risk as cuts to funding start to disrupt access to services for prevention, screening, and treatment for people with TB.
Those are just three of dozens of examples. In a news release today, StopTB Partnership Executive Director Lucica Ditiu, MD, echoed Tedros’s call for action.
“People with TB need us,” Ditiu said. “We have to remain strong, and we can never ever give up the fight. Through innovative, global and national efforts and standing together, we will be able to achieve these targets of ensuring TB prevention, treatment, and care are accessible to all.”
TB was responsible for an estimated 1.25 million deaths in 2023, according to the WHO’s most recent annual report. An estimated 8.2 million people were newly diagnosed with the disease—the most cases in a year recorded by the WHO since it began global TB monitoring in 1995. High-burden TB countries have only recently begun to recover from the disruptions caused by the COVID-19 pandemic, which the WHO estimates resulted in 700,000 excess TB deaths.
Cuts exacerbate funding shortfalls
As the WHO notes, the funding cuts come amid what was already a shortfall in funding for global TB control efforts. In 2023, $5.7 billion was available for TB prevention, diagnostic, and treatment services in low- and middle-income countries, but that’s only 26% of the 2027 target goal of $22 billion. TB research is receiving just one fifth of its 2022 target of $5 billion. Cuts to US funding are only going to exacerbate the problem.
In a joint statement issued earlier this week, Tedros and the Civil Society Task Force on Tuberculosis called on countries to take urgent action to prevent any disruption to TB services, ensure domestic resources to sustain equitable and essential TB care, and safeguard essential TB drugs, diagnostics, care, and social protection coverage for TB patients. They also urged the establishment of national partner platforms that would bring together public and private sectors, civil society, nongovernmental organizations, professional societies, and donors to maintain momentum against TB in affected countries.
“This urgent call is timely and underscores the necessity of swift, decisive action to sustain global TB progress and prevent setbacks that could cost lives,” said Tereza Kasaeva, PhD, director of WHO’s Global Programme on TB and Lung Health, in today’s WHO news release.
-

 News17 hours ago
News17 hours agoBLACK EASTER: Over 150 massacred in Plateau, Benue
-

 News13 hours ago
News13 hours agoDouble tragedy: Father, three children, maid killed in Osun road crash
-

 News13 hours ago
News13 hours agoSAD! SEC DG says “we can’t recover N1.3trn Nigerians lost to CBEX ponzi scheme”
-
 News11 hours ago
News11 hours agoNDLEA nabs bandits supplier with drugs concealed in private part(Photos)
-

 Metro16 hours ago
Metro16 hours agoShock as 2 naked lovers found dead in Kogi
-

 News17 hours ago
News17 hours agoIMF expresses concern over high poverty rate, food insecurity in Nigeria
-
 News12 hours ago
News12 hours agoNUJ-FCT Chairman Urges Journalists to Embrace Spirit of Easter
-

 Economy17 hours ago
Economy17 hours agoVolvo announces termination of 800 U.S. workers, cites tariff, market decline