Health
Women born with male, female sex organs can father children, says Gynaecologists
By Francesca Hangeior.
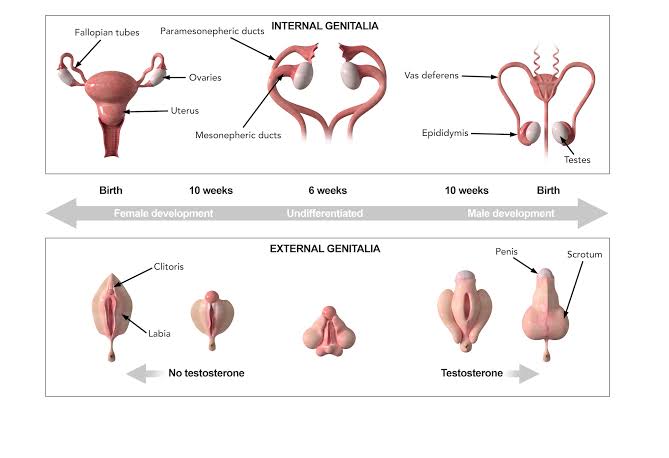
Senior obstetricians and gynaecologists have stated that individuals with female external features who were born with both male and female sexual organs (intersex) could father children.
The experts, however, clarified that this was possible in intersex females who have functional and developed male reproductive organs.
They noted that although such cases were rare, they were possible and had happened in medical history.
Their statement is coming on the heels of a recent interview with an intersex female, Queen Obukoko, who after failed relationships with men impregnated two women.
According to reports she had discovered a penile-like growth around her groin while growing up and had tried several things to ‘treat’ it.
Although Obukoko looks and has a female structure, she stated that she began to urinate through the male genitalia when she was 15 years old.
Obukoko further noted that she had trouble maintaining romantic relationships with men as they abandoned her whenever they discovered her condition.
After the failed relationships, the 30-year-old stated that she decided to have romantic relationships with women, which led to the birth of a son and daughter.
Although details of whether Obukoko knew a family member with such a condition were unclear, she hinted at the possibility of her newborn daughter being intersex.
According to the Cleveland Clinic, people who are intersex have a sexual and reproductive anatomy that does not fit into the exclusively male or female sex classification.
It added that although the intersex traits might be visible at birth, they were more pronounced during puberty and adulthood.
Also, it affirms that intersex is rare and only two per cent of people globally have the traits.
Cleveland Clinic also notes that intersex surgeries were often carried out before the child reached two years.
The confusion of parents of a 10-year-old intersex boy who after six correction surgeries, ended up with urinary incontinence and an unclear gender.
The experts explained intersex individuals could have partially functional sexual organs at birth.
The gynaecologists further noted that the dominant reproductive organ was more pronounced during puberty.
Providing clarifications on the issue, a former president of the Society of Gynaecology and Obstetrics of Nigeria, Professor Rotimi Akinola, stated that although rare, an intersex woman can impregnate another woman.
He explained that intersex individuals may possess both male and female reproductive organs that are developed and functional.
“It’s not impossible although it could be extremely rare. The reason it is not impossible is because there are some things they call mosaic. Mosaic is neither right nor left so you have both capabilities in the genital tract. It means that some cells in her body are in one line and the other in another line. The reason that you can be a hermaphrodite in the first place is the same reason why it depends on the organs and all those things.
“This is not a make-believe and it’s not the case of somebody who is trying to change sex. This is the genetic makeup and not a phenotype, like an appearance. It’s structurally so and she has both organs and they are all not rudimentary. So, to some extent, both can function,” the don said.
Akinola further stated that intersex females could have an ovary on one side and a testis on the other side.
He added that in Obukoko’s case, her physical appearance presented her as a woman but structurally, she could function as a man.
“Her appearance is such that she is better off as a woman. Yes. That’s the way she is made, that’s the way she will be accepted and that’s the way she grew up. But the fact remains that structurally she can function in another dimension,” the gynaecologist said.
Akinola, who practices at the Lagos State University Teaching Hospital, Ikeja, noted that Obukoko’s suspicion that her newborn daughter was intersex was valid as her condition was genetic and could be passed down to her children.
He further noted that undergoing intersex surgery was difficult for intersex adults because their sexual organs were fully developed, stating it was better done as a child.
“For her, it’s difficult because her sexual organs are all developed so it’s difficult to revert. She can start taking male hormones now and she’ll begin to grow a beard and then build muscles. That’s possible. But it’s going to be more difficult because of the acceptance that she has had in the past.
“But for a child, if it is confirmed, they can mask or obliterate one. In all human beings, the neutral expression of sex is female. If you don’t have androgens and testes, you will come out as a female, genetically.
“So when they talk about androgen insensitivity that is the person is not sensitive to the male hormones and such a person will come out in the neutral gender, which is female. So the neutral gender is female for both sexes,” the gynaecologist said.
He also hinted that Obukoko could get pregnant if she had a well-developed womb.
Also, the Second Vice president of SOGON, Professor Chris Aimakhu, explained that intersex is a condition in which a human being is born with reproductive or sexual organs that cannot be characterised as male or female.
He added that it was mainly caused by abnormalities in the genetic chromosomes that are not male or female.
The don also asserted that intersex persons could have partially functional sexual organs at birth, noting that as they grow the dominant reproductive organs are more pronounced.
He further noted that most of the time, intersex persons are present in the hospital during puberty.
“Usually at puberty is when they present to the hospital when the sexual characteristics do not develop. However, surgical correction can be done to correct the organs,” Aimakhu said.
Speaking on the characteristics of an intersex, the don said, “Having ambiguous genitalia at birth, a very small penis, an enlarged clitoris, partly fused labia (labia is the inner, labia minora, and outer folds, labia majora, that forms the skin folds that protects the opening of the urethra and vagina), undescended testis that may eventually turn out to be ovaries in a male intersex and a labial or groin mass that may turn out to be testes in female intersex.”
Health
FG identifies 1,277 persons for monitoring as Lassa fever kills 122

The Nigeria Centre for Disease Control and Prevention has listed 1,277 persons for follow-up over the possibility of being infected with Lassa fever. This follows the centre recording 659 confirmed cases out of 3,779 suspected cases and 122 deaths in 13 weeks (from January to March 30, 2025).
A report obtained from the NCDC on Friday indicated that no fewer than 18 states across the country have recorded Lassa fever cases, with Ondo, Bauchi, and Edo being the most affected.
The report partly reads, “Cumulatively, in week 13 of 2025, 122 deaths have been reported, with a Case Fatality Rate of 18.5%, which is lower than the CFR for the same period in 2024 (18.7%).
“In total for 2025, 18 states have recorded at least one confirmed case across 93 Local Government Areas. Seventy-one per cent of all confirmed Lassa fever cases were reported from these three states (Ondo, Bauchi, and Edo), while 29% were reported from 15 other states with confirmed Lassa fever cases. Of the 71% of confirmed cases, Ondo reported 30%, Bauchi 25%, and Edo 16%.
“The predominant age group affected is 21-30 years (Range: 1 to 94 years, Median Age: 30 years). The male-to-female ratio for confirmed cases is 1:0.8. The number of suspected cases increased compared to that reported for the same period in 2024. No new healthcare worker was affected in week 13. The National Lassa fever multi-partner, multi-sectoral Incident Management System (IMS) was activated to coordinate the response activities at all levels.”
The report shows that the contacts under follow-up number 1,277, while the contacts that have completed follow-up total 1,448.
According to the NCDC, the disease has affected 20 healthcare workers in eight states so far this year.
Lassa fever is an acute viral haemorrhagic fever caused by the Lassa virus. The natural reservoir for the virus is the multimammate rat (also known as the African rat), although other rodents can also act as carriers.
The public health institute stated that Lassa fever cases occur year-round, with peak transmission periods typically from October to May.
Health
WHO calls for countries to address disruptions to TB services
In the wake of massive cuts in US funding, the World Health Organization (WHO) today called on global health leaders, donors, and policymakers to protect and maintain tuberculosis (TB) care and support services around the world.
In a statement issued ahead of World Tuberculosis Day (March 24), the WHO said the “drastic and abrupt” cuts to global health funding threaten to reverse gains made in global efforts to combat TB, which remains the world’s deadliest infectious disease. Those efforts have saved an estimated 79 million lives worldwide since 2000, the organization said.
“The huge gains the world has made against TB over the past 20 years are now at risk as cuts to funding start to disrupt access to services for prevention, screening, and treatment for people with TB,” said WHO Director-General Tedros Adhanom Ghebreyesus, PhD. “But we cannot give up on the concrete commitments that world leaders made at the UN General Assembly just 18 months ago to accelerate work to end TB. WHO is committed to working with all donors, partners and affected countries to mitigate the impact of funding cuts and find innovative solutions.”
USAID cuts have crippled TB control efforts
While the statement does not specifically mention the US Agency for International Development (USAID), the Trump administration’s freeze of USAID funding, and the subsequent canceling of thousands of contracts issued by the agency, have left a gaping hole in funding for TB prevention, screening, and treatment services. The US government has been the leading bilateral donor to global TB control efforts, contributing $200 million to $250 million annually—roughly one quarter of international donor funding for the disease.
The WHO said 27 countries are facing crippling breakdowns in their TB response, with the biggest impact seen in high-TB burden countries in Africa, Southeast Asia, and the Western Pacific. Among the services that have been disrupted are diagnosis, active case finding, screening, and contact tracing, and those disruptions are resulting in delayed detection and treatment and increased transmission risk. Drug supply chains, laboratory services, and data and surveillance systems have also been undermined.
A recent update from StopTB Partnership, which works on TB response with more than 2,000 partners in 100 countries, provides some detail on the services affected by the USAID funding cuts. In Cambodia, active case finding has halted in half the country, resulting in 100,000 people missing TB screening and 10,000 cases of drug-susceptible (DS)-TB going undetected. In Kenya, sputum sample transport once supported by USAID has halted, affecting the diagnosis of DS- and drug-resistant (DR)-TB. In India, USAID-funded TB screening projects in vulnerable groups have stopped.
The huge gains the world has made against TB over the past 20 years are now at risk as cuts to funding start to disrupt access to services for prevention, screening, and treatment for people with TB.
Those are just three of dozens of examples. In a news release today, StopTB Partnership Executive Director Lucica Ditiu, MD, echoed Tedros’s call for action.
“People with TB need us,” Ditiu said. “We have to remain strong, and we can never ever give up the fight. Through innovative, global and national efforts and standing together, we will be able to achieve these targets of ensuring TB prevention, treatment, and care are accessible to all.”
TB was responsible for an estimated 1.25 million deaths in 2023, according to the WHO’s most recent annual report. An estimated 8.2 million people were newly diagnosed with the disease—the most cases in a year recorded by the WHO since it began global TB monitoring in 1995. High-burden TB countries have only recently begun to recover from the disruptions caused by the COVID-19 pandemic, which the WHO estimates resulted in 700,000 excess TB deaths.
Cuts exacerbate funding shortfalls
As the WHO notes, the funding cuts come amid what was already a shortfall in funding for global TB control efforts. In 2023, $5.7 billion was available for TB prevention, diagnostic, and treatment services in low- and middle-income countries, but that’s only 26% of the 2027 target goal of $22 billion. TB research is receiving just one fifth of its 2022 target of $5 billion. Cuts to US funding are only going to exacerbate the problem.
In a joint statement issued earlier this week, Tedros and the Civil Society Task Force on Tuberculosis called on countries to take urgent action to prevent any disruption to TB services, ensure domestic resources to sustain equitable and essential TB care, and safeguard essential TB drugs, diagnostics, care, and social protection coverage for TB patients. They also urged the establishment of national partner platforms that would bring together public and private sectors, civil society, nongovernmental organizations, professional societies, and donors to maintain momentum against TB in affected countries.
“This urgent call is timely and underscores the necessity of swift, decisive action to sustain global TB progress and prevent setbacks that could cost lives,” said Tereza Kasaeva, PhD, director of WHO’s Global Programme on TB and Lung Health, in today’s WHO news release.
Health
Women with VVF can have normal s3xual lives after treatment, say gynaecologists

By Francesca Hangeior
After proper surgical repair, women who have a vesicovaginal fistula, an abnormal opening between the bladder and the vaginal wall, leading to urine leakage and other complications, can have a pleasurable sexual life, gynaecologists have assured.
They advised such women to wait until 12 weeks after the surgery to allow complete healing and recovery before resuming sexual activities.
The maternal experts, however, stated that the return to normal sexual life depended on the delays before the repair was done and the scarred tissues that were formed, stating that some of the women might experience vagina tightness and pain during sex.
The fertility experts further emphasised the need for counselling and psychotherapy before resuming sexual activity, to ensure that the fear, anxiety, and emotional trauma related to sex and pregnancy were overcome.
According to the seasoned obstetric gynaecologists, women with repaired VVF, who desired more children, could become pregnant and have more babies.
However, they stressed that such delivery must be through a caesarean section and done in a conventional health facility.
VVF is a complication of obstructed labour during delivery. According to the United Nations Population Fund, VVF is a major public health problem with over two million cases, globally.
In Nigeria, there are about 150,000 cases with 12,000 new cases recorded every year.
Many women with VVF in Nigeria battle with stigma, leading to social ostracisation, abandonment, and psychological distress.
Also, a professor of Obstetrics and Gynaecology at the Usmanu Danfodiyo University, Abubakar Panti, stated that after the successful closure of the fistula and complete healing after surgery, normal sexual activity could be restored.
He further stated that to ensure proper healing and recovery time, the recommendation was to avoid sexual activity for at least three months, which is 12 weeks post-surgery to allow complete healing.
The don also stated that before resuming sexual activity, the strength of the pelvic floor must be assessed, as some women may experience vaginal tightness or weakness after prolonged fistula, which could affect sexual comfort.
To resolve this, Panti advised the women to do some pelvic floor exercises, noting that sometimes the help of a physiotherapist was needed.
“When women have lived with VVF for a long time, they know what caused it, they know it’s a pregnancy that caused it, so they may experience fear, anxiety or some form of emotional trauma related to sex, because they would think sex is what brought it in the first place, so they need a lot of counselling or therapy, in that instance psychotherapy may be beneficial.
“Some of these women used to have a lot of terrible experiences, sometimes they are abandoned by their husbands, divorced and other things, so they think every man may be like that.
“The last one probably would be the presence of scarring or vaginal shortening. If extensive damage occurred before repair, some women may have vaginal scarring and then sometimes there will be dryness of the vagina or reduced elasticity.
“Usually, the vagina distends to accommodate, irrespective of the size of the penis that comes into it, so if there is scarring, that distension will not be there, and there will be tightness, so this can also affect comfort during sex. Most of the time we just tell them to apply lubricants and sometimes medical interventions may help,” the fertility expert said.
Panti asserted that with successful surgery, proper healing and emotional support, many women regained a satisfying sexual life.
He advised the women to whenever they had concerns or difficulties, consult their gynaecologist, who would give them tips regarding the repair, sexual health and resuming sexual activity.
Panti emphasised the need for counselling the woman and her husband, “because it needs a lot of patience from the partner, that he has to start slow and of course, he has to listen to her or look at her body language if she’s in any discomfort or experiencing pain so that he can stop, rest and try again.”
The don advised the women to watch out for symptoms like leakage of urine and consult with the gynae if there’s discomfort during sex.
The consultant gynaecologist urged them to focus on their overall wellness by eating well and preventing urinary tract infections.
“With proper healing, patience and emotional support, most of them regain their full sexual life after VVF repair, the key is to slow down, communicate with your partner and seek medical advice where needed,” Panti said.
He further stated subsequent delivery after VVF must be by caesarean section, to prevent a reopening of the repair.
-
 News7 hours ago
News7 hours agoSHOCKING! One month after giving birth, woman discovers another baby in her womb
-

 News8 hours ago
News8 hours agoTears, anguish as Plateau Community buries 51 killed by bandits
-

 News14 hours ago
News14 hours agoPeter Obi speaks as Benue govt. blocks humanitarian visit
-

 News7 hours ago
News7 hours agoAngry investors raid CBEX office, loot assets in Ibadan after digital Platform crash
-

 News14 hours ago
News14 hours agoFUOYE VC suspended over sexual harassment allegations
-

 News7 hours ago
News7 hours ago‘Not something I’d wish on anyone’ — Melinda Gates opens up on divorce
-

 News5 hours ago
News5 hours agoCBEX: 60 fraudulent Ponzi scheme operators to avoid in Nigeria
-

 Politics7 hours ago
Politics7 hours agoIgbo Youths Set To Mobilize 5 Million Man-March In Support Of Tinubu, Kalu